- Membership Resources
- State Chapters
- Education/Events
-
Advocacy/Policy
- Home Care Workforce Crisis: An Industry Report and Call to Action
- Advocacy Fund
- State of Home Care: Industry at Crossroads
- Home Care Workforce Action Alliance
- Caring for Seniors: Value of Home Care
- Home Care by the Numbers
- Issues & Positions
- Legislative Action Network
- State Legislation Tracker
- Federal Legislation Tracker
- 2024 National Advocacy Day
- About HCAOA
- Find a Job
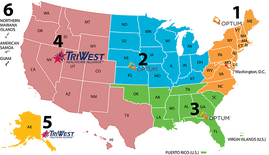 HCAOA has an update for members providing care under the VA Community Care Network. Effective June 9, TriWest began subcontracting all VACCN Region 4 health care claims processing and payment with PGBA. However, due to various technical issues on PGBA’s end, the first post-transition payments didn’t go out from PGBA until the week of July 12. “HCAOA members may have received a number of denials for June claims, but TriWest and PGBA are currently working to resolve those issues. Other than the June discrepancies, payments appear to be flowing correctly,” reported Doug Robertson, Chair of HCAOA’s Veteran Services Council. HCAOA continues to maintain contact with TriWest leadership on the transition status. Providers who continue to encounter issues with TriWest can email the new claim support address: [email protected], which is monitored by a team at TriWest. When submitting a claim, be sure to include: Veteran name, DOB, SSN, and dates of service in question in an excel report to get an investigation started. Use a secure email service when sending veteran PHI.
Additionally, TriWest will be launching Availity Plus (an Availity upgrade) on September 18. HCAOA will provide more information on that release in the Fall.
1 Comment
7/28/2021 12:21:20 pm
Tri-West has paid short all of our invoices from January-June. We are using the VA Fee Schedule that vary from county. They are paying the lesser amount for the wrong county.
Reply
Leave a Reply. |
Archives
July 2024
Categories
All
Upcoming Events |
|
Phone: 202-519-2960 | 444 N. Capitol Street NW, Suite 428 | Washington, DC 20001
[email protected] | sitemap © 2024 Home Care Association of America. All Rights Reserved. | Privacy Policy | Refund Policy |
|

 RSS Feed
RSS Feed